Advances in IOL optics, materials, and technology are reducing patients’ reliance on glasses after cataract surgery,1,2 thereby improving their overall quality of life. Optometrists play a vital role in patient education, candidate selection, and postoperative management. Having a comprehensive understanding of current lens offerings allows ODs to provide better guidance on postoperative expectations and trade-offs and, as a result, increase patients’ long-term satisfaction.
This article explores available premium IOL categories, including monofocal plus, extended depth of focus (EDOF), multifocal, light adjustable, and small aperture.
MONOFOCAL PLUS IOLs
This emerging category of IOLs is designed to provide a modest extension of depth of focus compared with standard monofocal lenses, with the goal of improving patients’ uncorrected intermediate visual acuity (UIVA).3-5 For example, the Tecnis Eyhance (Johnson & Johnson Vision) is a hydrophobic acrylic one-piece IOL that features +0.50 D of added central power and negative spherical aberration (Figure 1A). The Eyhance can be a good choice for patients who have a history of myopic LASIK. Not only does the lens counteract the positive corneal spherical aberration typically found in these eyes, but the increased range of focus the IOL provides also theoretically makes it more tolerant of minor postoperative refractive errors compared with a standard monofocal. The RayOne EMV (Rayner) offers similar advantages for this patient population. This one-piece hydrophilic acrylic IOL has a positive spherical aberration design and provides up to 1.50 D of increased range of focus and thus could be a good choice for patients with a history of hyperopic LASIK (Figure 1B).6-8
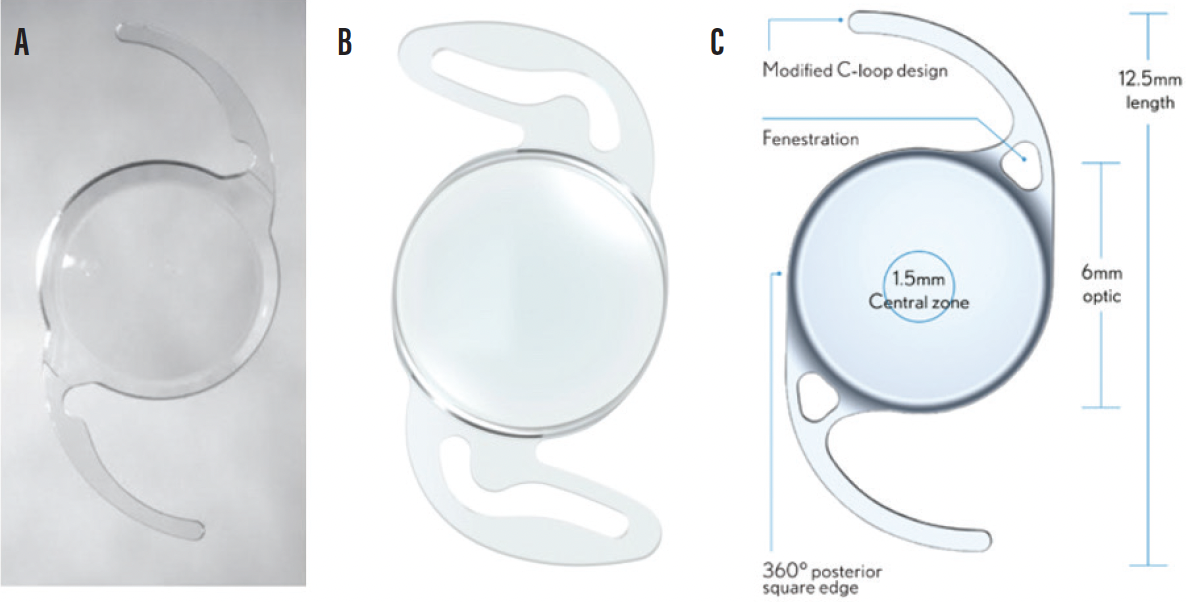
Figure 1. The Tecnis Eyhance (A), RayOne EMV (B), and enVista Aspire (C).
Images courtesy of Johnson & Johnson Vision, Rayner, and Bausch + Lomb.
The enVista Aspire (Bausch + Lomb) is a hydrophobic acrylic, aberration-neutral, one-piece IOL that features an intermediate-optimized central zone designed to provide 1.25 D of continuous depth of focus (Figure 1C). The Light Adjustable Lens Plus (LAL+; RxSight) also fits in this category and is further discussed later in this article.
Surgeons may use a monovision or mini monovision strategy with a monofocal plus lens to reduce patients’ spectacle dependence by slightly undercorrecting their nondominant eye.4,7,9 Although neither strategy can eliminate a patient’s need for reading glasses postoperatively, each offers a compromise to individuals seeking some degree of UIVA.
EXTENDED DEPTH OF FOCUS IOLS
As the midway point between standard monofocal IOLs and multifocal IOLs, EDOF IOLs enhance patients’ UIVA while providing some functional near vision. The lenses on the US market that meet the American National Standards Institute’s criteria for an EDOF IOL are the Tecnis Symfony (Johnson & Johnson Vision) and Clareon IQ Vivity (Alcon). Both provide about 1.50 D of added intermediate range of vision (Figure 2). The IC-8 Apthera lens (Bausch + Lomb) meets the same criteria and is discussed later in this article in the section on small-aperture IOLs. The Symfony is a diffractive lens with an echelette design (ie, successive rings that split light into a wider range). The Vivity is a refractive lens with a unique change in curvature in its central 2.2-mm zone that elongates the patient’s focal range.
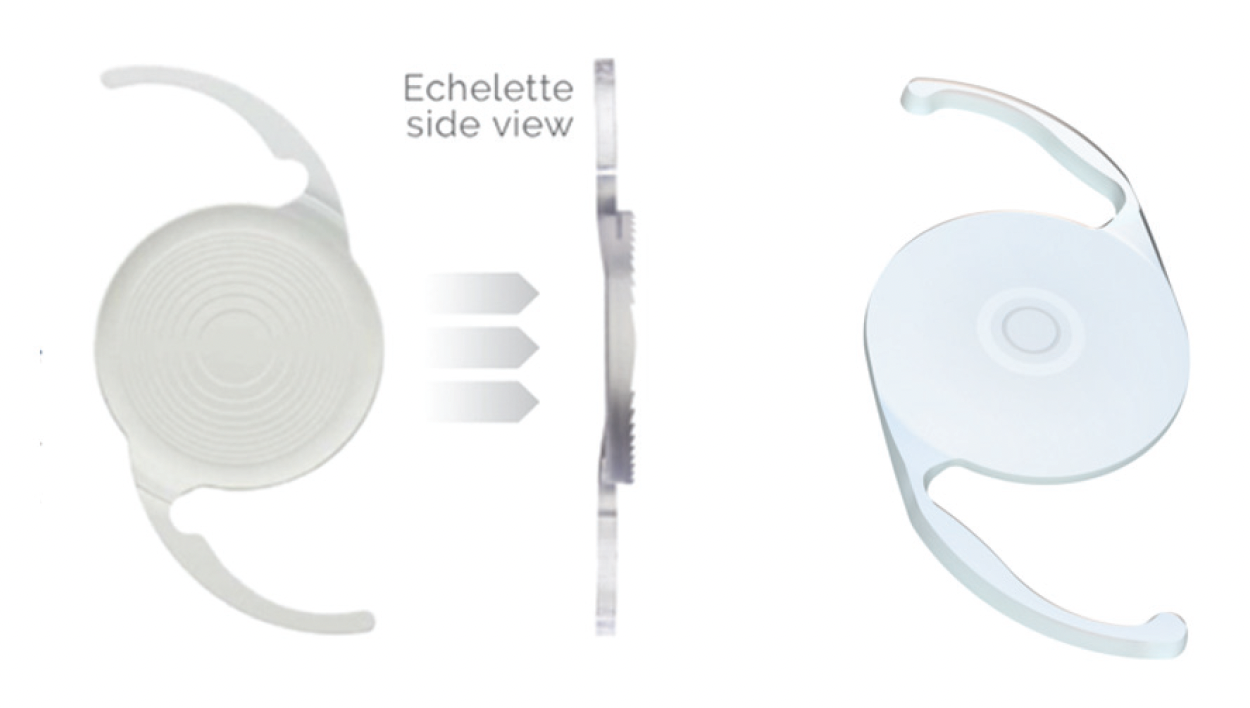
Figure 2. The Tecnis Symfony (A) and Clareon IQ Vivity (B).
Images courtesy of Johnson & Johnson Vision and Alcon.
It is important to note that EDOF lenses are not without visual side effects. Although EDOF IOLs are designed to minimize glare and halos compared with multifocal lenses, some patients who receive EDOF IOLs report these visual phenomenona.10,11
MULTIFOCAL IOLs
Like bifocal and trifocal glasses, multifocal IOLs are designed to provide patients with functional near, intermediate, and distance vision, and individuals who receive these lens implants can achieve high rates of spectacle independence (≥ 80%).12
Multifocal IOLs available in the United States include the Clareon PanOptix Pro (Alcon), enVista Envy (Bausch + Lomb), and Tecnis Odyssey (Johnson & Johnson Vision; Figure 3). The PanOptix Pro is a hydrophobic acrylic trifocal diffractive IOL that uses concentric rings to split light across three focal points. The Envy is a hydrophobic acrylic, nondiffractive, aberration-neutral trifocal IOL that uses wavefront-shaping technology to provide vision at all three focal points. The Odyssey is a nondiffractive hybrid IOL that blends EDOF and multifocal technology to extend patients’ range of vision.
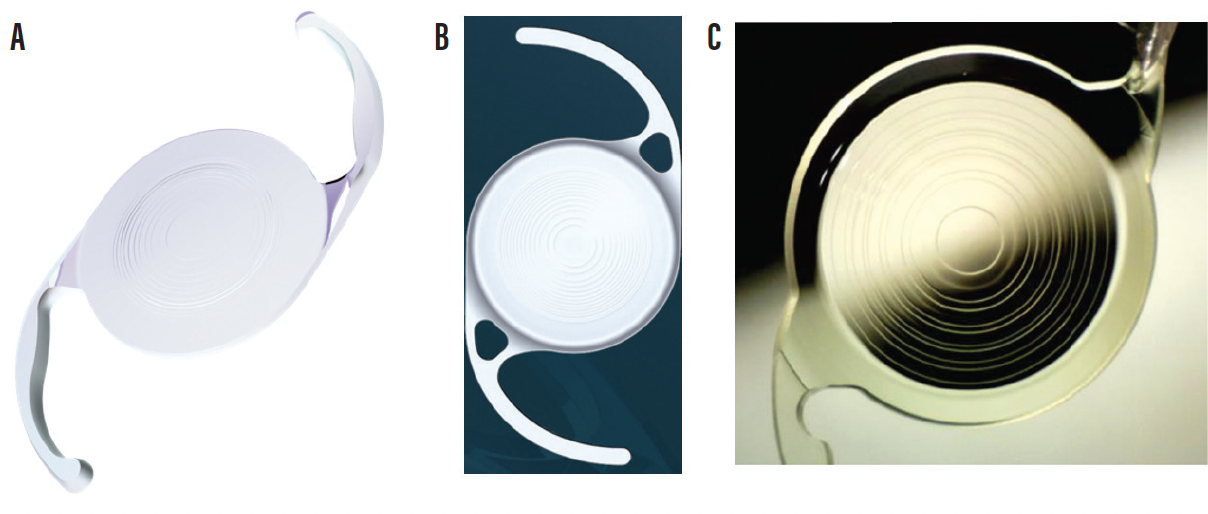
Figure 3. The Clareon PanOptix Pro (A), enVista Envy (B), and Tecnis Odyssey (C).
Images courtesy of Alcon, Bausch + Lomb, and Johnson & Johnson Vision.
The well-known tradeoffs of multifocal IOLs include glare, halos, and reduced contrast sensitivity in low-light settings, making these lenses less suitable for patients with high night vision demands (eg, drivers and pilots). Several studies found that monofocal IOLs outperformed multifocal lenses in this area.13-15 Large pupils may increase glare and halos with multifocal IOLs. Despite potential optical side effects, overall patient satisfaction and quality of life with this category of lenses are high.12
Careful patient selection is essential. Preexisting ocular comorbidities such as corneal dystrophy (eg, Fuchs and epithelial basement dystrophy), pterygia, optic nerve damage (eg, glaucoma), and retinal pathology (eg age-related macular degeneration, diabetic maculopathy, and epiretinal membrane) merit careful assessment because of the potential for progression.16 Ocular surface disease, especially dry eye and meibomian gland dysfunction, should be treated preoperatively.16
Another concern with multifocal lens implants is that they can impede visualization of the macula and optic nerve, which could negatively affect the diagnosis and management of posterior segment disease.
Patients with higher-order aberrations from prior refractive surgery are generally poor candidates for a multifocal IOL.16 In this situation, a monofocal lens or monovision strategy may be a better option for reducing their spectacle dependence after cataract surgery. It is also worth noting that advanced-technology IOLs with sophisticated optics (including both toric and multifocal designs) are sensitive to decentration and rotation.12 Capsular instability from pseudoexfoliation or zonulopathy or a large angle kappa can compromise the performance of these IOLs.
LIGHT ADJUSTABLE LENsES
The LAL is the only lens implant available that can be adjusted postoperatively to fine-tune the patient’s refractive outcome (Figure 4). The LAL can correct up to 2.00 D of sphere and 2.00 D of astigmatism after it is implanted, making it especially useful for patients whose preoperative measurements may be inaccurate owing to prior refractive surgery, corneal irregularity, or severe ocular surface disease. Approximately 88% of eyes with a history of refractive surgery have achieved 20/25 UCVA or better.17
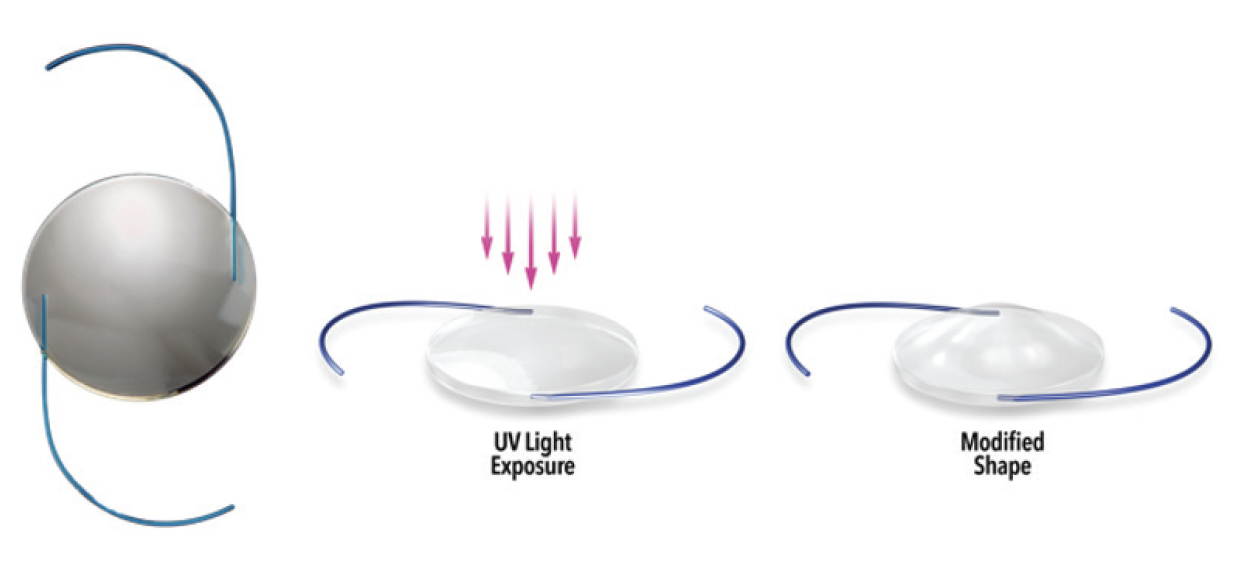
Figure 4. The LAL.
Images courtesy of Rx Sight.
LALs are commonly used with a monovision strategy to broaden patients’ functional vision. In one study, 96% of patients achieved 20/20 distance and J2 near visual acuity.18 Unlike multifocal lenses, LALs do not split light; therefore, patients do not experience glare and halos.
The LAL+ features a continuous central power gradient that modestly extends depth of focus without compromising distance clarity. A common surgical strategy is to implant an LAL in the dominant eye and an LAL+ in the nondominant eye to enhance the patient’s range of vision. The LAL+, however, should be used cautiously in patients who have a history of refractive surgery owing to the risk of induced aberrations.
SMALL-APERTURE IOLs
IOLs such as the IC-8 Apthera use pinhole optics to extend depth of focus and reduce glare (Figure 5). Although classified as EDOF lenses, small-aperture IOLs have a unique mechanism of action that may be especially beneficial to eyes for which multifocal optics are contraindicated. A central opaque ring limits peripheral aberrations and enhances depth of focus. Thus, these lenses can be an excellent choice for patients with higher-order aberrations or irregular corneas such as from keratoconus.
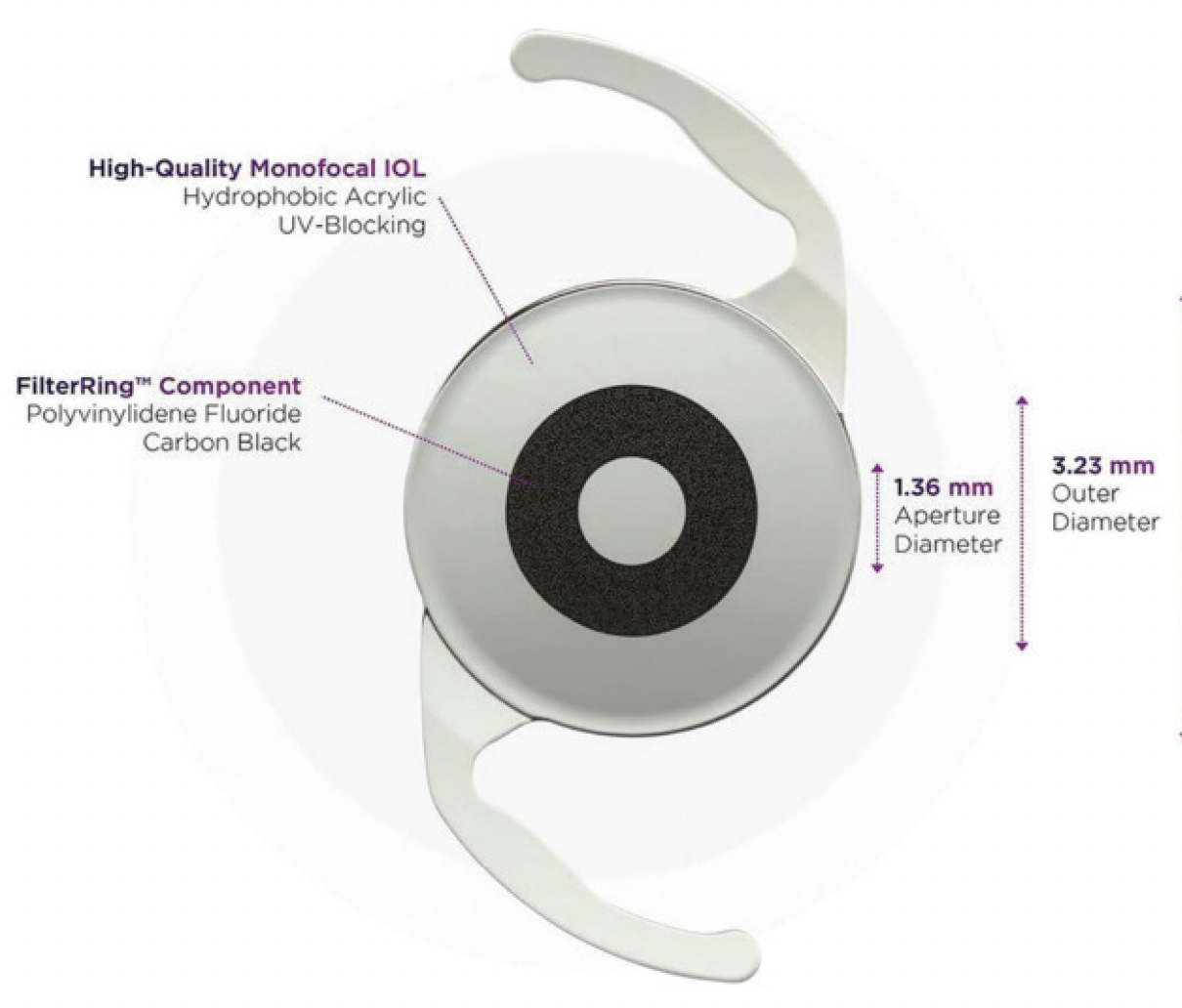
Figure 5. The IC-8 Apthera.
Image courtesy of Bausch + Lomb.
A lot of incoming light is lost with small-aperture IOLs, which can be bothersome in low-light conditions. These lenses are therefore typically implanted unilaterally in the patient’s nondominant eye, with a monofocal IOL implanted in the fellow eye so the patient maintains crisp distance vision.
PERSONALIZE YOUR RECOMMENDATIONS
No one IOL is ideal for every patient. Each lens design involves trade-offs, many related to the fundamental challenge of splitting light. Strategically combining different types of IOLs can improve patients’ binocular visual outcomes at different distances.19 Blended vision approaches combine multifocal, EDOF, or monofocal lenses to optimize binocular vision across all focal points.9,20 Excellent results have been reported with this strategy; in one study, up to 99% of patients achieved a binocular visual acuity of 0.03 logMAR.14 Successful outcomes with premium IOLs begin with proper patient selection and comprehensive preoperative counseling.16 Ideal candidates are motivated to achieve spectacle independence, understand the potential trade-offs of each technology, and have realistic expectations.
As novel IOL materials, more sophisticated designs, and AI-guided selection tools are developed, vision correction becomes increasingly personalized. By staying current on emerging technologies, educating patients effectively, and collaborating closely with surgeons, optometrists can help deliver optimal outcomes and elevate the standard of care.
1. Zvorničanin J, Zvorničanin E. Premium intraocular lenses: the past, present and future. J Curr Ophthalmol. 2018;30(4):287-296.
2. Grzybowski A, Kanclerz P. Recent developments in cataract surgery. In: Grzybowski A, ed. Current Concepts in Ophthalmology. Springer; 2020:55-97.
3. Wan KH, Au ACK, Kua WN, et al. Enhanced monofocal versus conventional monofocal intraocular lens in cataract surgery: a meta-analysis. J Refract Surg. 2022;38(8):538-546.
4. Min H, Ambati B. Design and visual outcomes of enhanced monofocal IOLs. Cataract & Refractive Surgery Today. November/December 2024. Accessed June 3, 2025. https://crstoday.com/articles/nov-dec-2024/design-and-visual-outcomes-of-enhanced-monofocal-iols
5. Mencucci R, Cennamo M, Venturi D, Vignapiano R, Favuzza E. Visual outcome, optical quality, and patient satisfaction with a new monofocal IOL, enhanced for intermediate vision: preliminary results. J Cataract Refract Surg. 2020;46(3):378-387.
6. Schmid R, Fuchs C, Luedtke H, Borkenstein AF. Depth of focus of four novel extended range of vision intraocular lenses. Eur J Ophthalmol. 2023;33(1):257-261.
7. García-Bella J, Burgos-Blasco B, Vidal-Villegas B, Garzón N, Villanueva C, García-Feijoo J. Visual and refractive outcomes after bilateral implantation of an enhanced monofocal intraocular lens: prospective study. J Cataract Refract Surg. 2024;50(6):585-590.
8. Law EM, Aggarwal RK, Buckhurst PJ. Visual outcomes, contrast sensitivity, and defocus profile with an aspheric monofocal intraocular lens using positive spherical aberration. J Cataract Refract Surg. 2025;51(5):394-398.
9. Zeilinger J, Kronschläger M, Schlatter A, et al. Comparing an advanced monofocal with a non-diffractive extended depth of focus intraocular lens using a mini-monovision approach. Am J Ophthalmol. 2025;271:86-95.
10. Cho JY, Won YK, Park J, et al. Visual outcomes and optical quality of accommodative, multifocal, extended depth-of-focus, and monofocal intraocular lenses in presbyopia-correcting cataract surgery: a systematic review and Bayesian network meta-analysis. JAMA Ophthalmol. 2022;140(11):1045-1053.
11. Karam M, Alkhowaiter N, Alkhabbaz A, et al. Extended depth of focus versus trifocal for intraocular lens implantation: an updated systematic review and meta-analysis. Am J Ophthalmol. 2023;251:52-70.
12. Alio JL, Plaza-Puche AB, Férnandez-Buenaga R, Pikkel J, Maldonado M. Multifocal intraocular lenses: an overview. Surv Ophthalmol. 2017;62(5):611-634.
13. Wang SY, Stem MS, Oren G, Shtein R, Lichter PR. Patient-centered and visual quality outcomes of premium cataract surgery: a systematic review. Eur J Ophthalmol. 2017;27(4):387-401.
14. Rosen E, Alió JL, Dick HB, Dell S, Slade S. Efficacy and safety of multifocal intraocular lenses following cataract and refractive lens exchange: metaanalysis of peer-reviewed publications. J Cataract Refract Surg. 2016;42(2):310-328.
15. de Vries NE, Webers CA, Touwslager WR, et al. Dissatisfaction after implantation of multifocal intraocular lenses. J Cataract Refract Surg. 2011;37(5):859-865.
16. Braga-Mele R, Chang D, Dewey S, et al; ASCRS Cataract Clinical Committee. Multifocal intraocular lenses: relative indications and contraindications for implantation. J Cataract Refract Surg. 2014;40(2):313-322.
17. Jones M, Terveen DC, Berdahl JP, Thompson V, Kramer BA, Ferguson TJ. Clinical outcomes of the light-adjustable lens in eyes with a history of prior corneal refractive surgery. J Cataract Refract Surg. 2024;50(9):936-941.
18. Jun JH, Lieu A, Afshari NA. Light adjustable intraocular lenses in cataract surgery: considerations. Curr Opin Ophthalmol. 2024;35(1):44-49.
19. Breyer DRH, Kaymak H, Ax T, Kretz FTA, Auffarth GU, Hagen PR. Multifocal intraocular lenses and extended depth of focus intraocular lenses. Asia Pac J Ophthalmol (Phila). 2017;6(4):339-349.
20. Can İ, Bayhan HA. Clinical outcomes of enhanced monofocal (mono-EDOF) intraocular lenses with the mini-monovision technique versus trifocal intraocular lenses: a comparative study. Turk J Ophthalmol. 2024;54(4):190-197.
Ready to Claim Your Credits?
You have attempts to pass this post-test. Take your time and review carefully before submitting.
Good luck!



