This Case Report is Interactive!
Strengthen your understanding of geographic atrophy by answering the challenge questions below.
Case Presentation
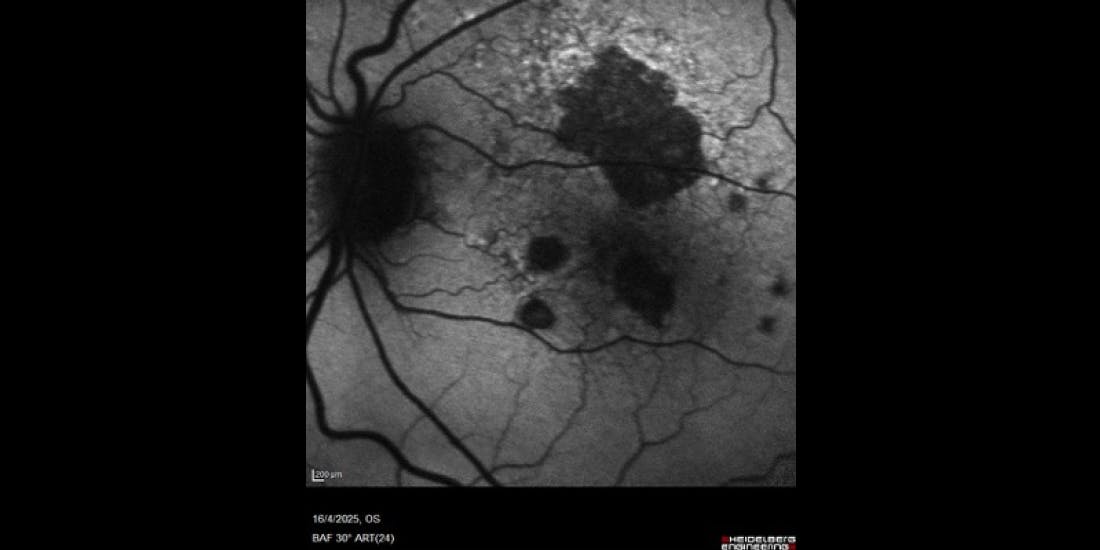
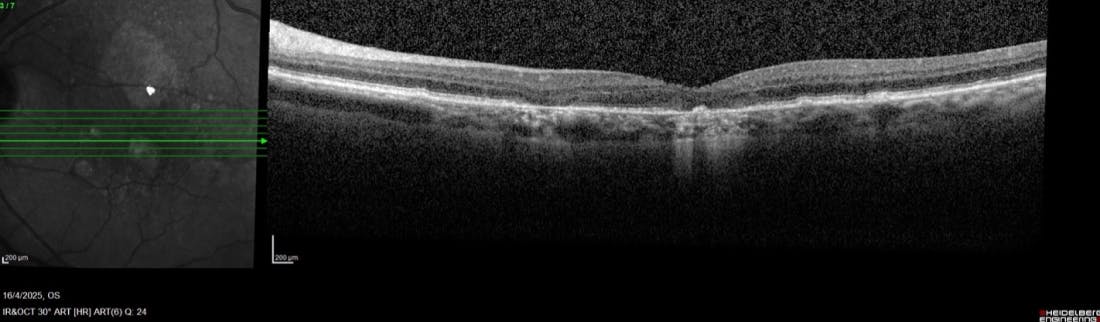
A 73-year-old woman was evaluated in our clinic in October 2018. At the time of the visit, the right eye was being treated for wet age-related macular degeneration (AMD) with quarterly intravitreal anti-VEGF injections. The left eye showed pigmentary changes, drusen, and normal foveal contour with no signs of atrophy (Figures 1 and 2).
- The patient was a non-smoker.
- She was not taking any medications and was living a healthy lifestyle.
- BCVA was 43 letters OD and 82 letters OS.
- The patient had no complaints about her vision in her left eye.
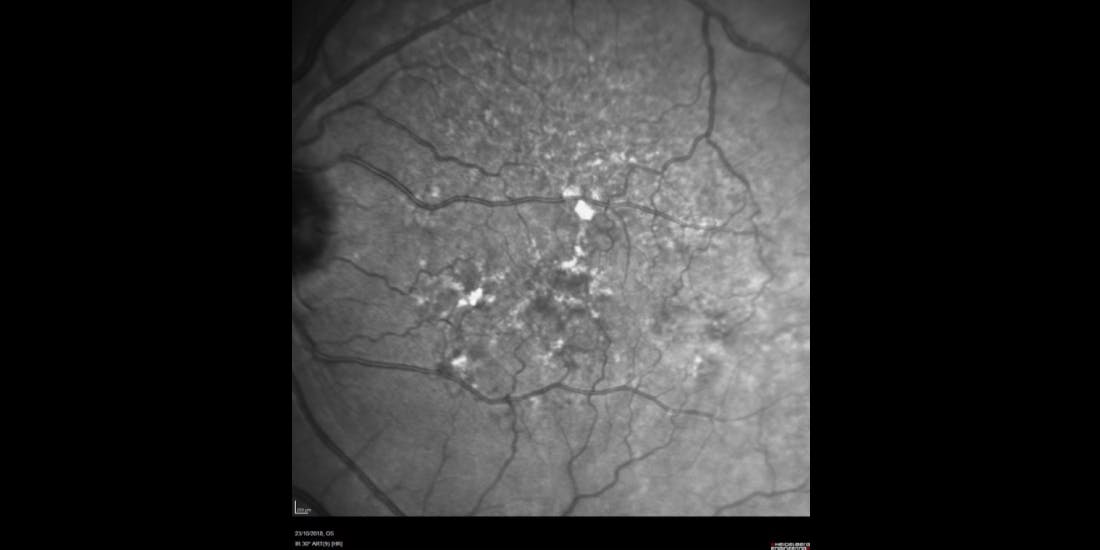
Figure 1. Near-infrared reflectance image of a left eye of a 73-year-old woman captured in October 2018 showing pigmentary changes and drusen.
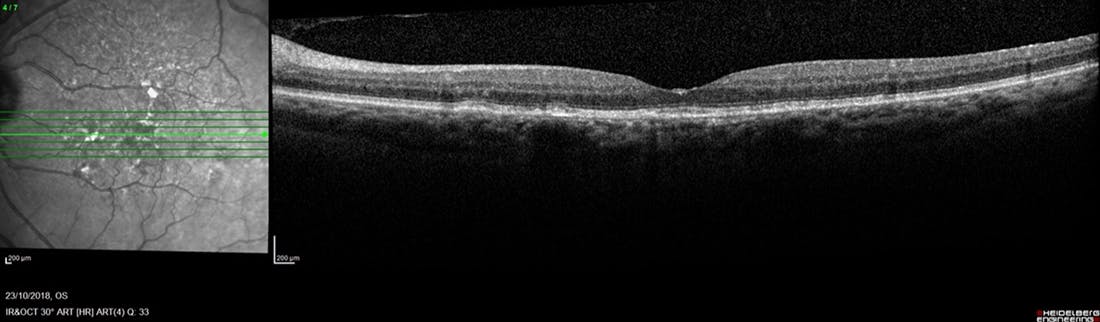
Figure 2. OCT of the same eye as shown in Figure 1 showing normal foveal contour and no signs of atrophy.
Challenge Question 1/2
All the following are good ways to evaluate functional vision in patients with geographic atrophy, EXCEPT:
Answer the question above to reveal more case details.


Answer: D. logMAR chart
The patient was seen again in March 2023 after she had been living abroad for 5 years. No imaging had been obtained in the interim. The right eye was still under treatment for wet AMD with good anatomical response. The patient was now complaining of worsening vision in the left eye. BCVA measured 80 letters OS; low luminance visual acuity was 46 letters OS. Fundus autofluorescence (FAF) showed scattered areas of atrophy around the fovea (Figure 3). The need for more frequent follow-up to obtain imaging to evaluate the speed of progression was discussed with the patient. As well, she was advised to contact us if there were any sudden changes in vision (such as conversion to wet AMD). Finally, the patient was educated about her prognosis, specifically that she has a progressive condition and that the large drop in BCVA under low luminance indicated poor contrast sensitivity. Indeed, although the BCVA had declined only 2 letters from the previous visit, it was highly likely that the subjective complaints of much worse vision were attributable to poor contrast sensitivity.
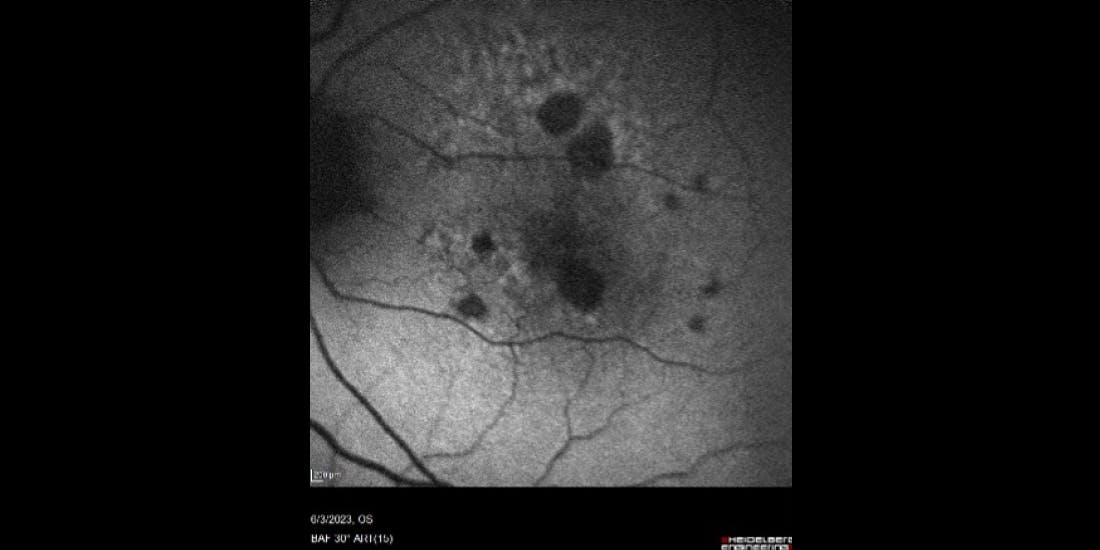
Figure 3. Blue autofluorescence taken in March 2023 showing scattered areas of atrophy around the fovea.
Challenge Question 2/2
Which of the following describes the most typical growth pattern associated with geographic atrophy lesions?


Answer: B. Lesions usually appear first outside the fovea, growing faster toward the periphery than toward the fovea.
The patient was next seen in our clinic in August 2024:
- Visual acuity had started to deteriorate: BCVA was 74 letters OS; low-luminance visual acuity was 32 letters OS.
- Patient complained of severe visual symptoms, although she stated that she was still maintaining an active and independent lifestyle.
-
FAF showed progression of areas of atrophy compared to the prior visit
(Figure 4).
- Enlargement of the atrophy was mostly away from the fovea.
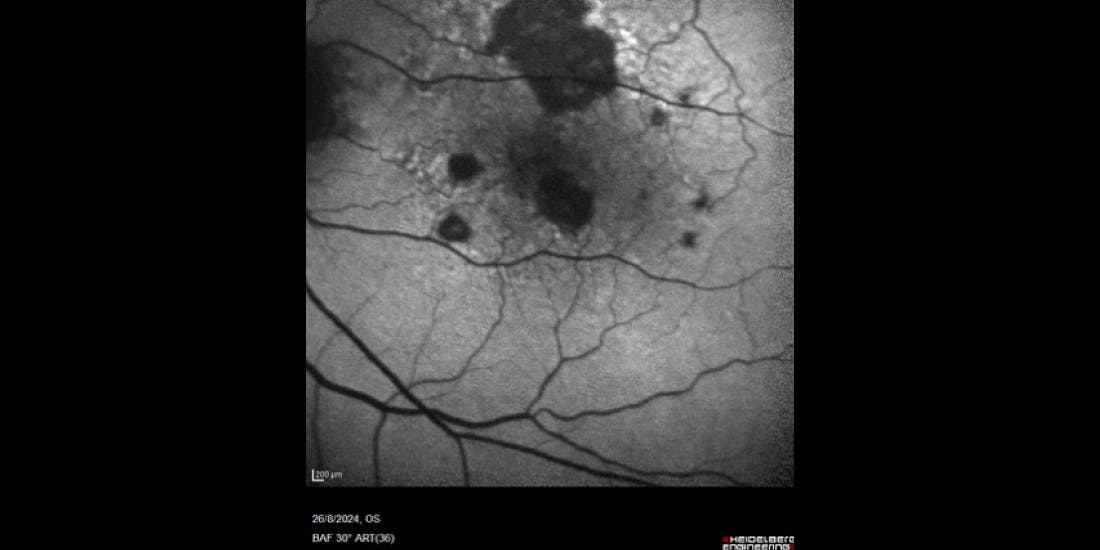
Figure 4. Fundus autofluorescence of the left eye of the patient in August 2024. Note the enlargement of atrophic areas compared to the prior visit (shown in Figure 3), largely due to coalescing of lesions.
Treatment options were discussed with the patient. Although anti-complement drugs are not yet available in our country, the patient expressed a willingness to start treatment to prevent further vision loss.
The most recent follow-up with this patient was in April 2025:
- Vision had further deteriorated: BCVA was 65 letters OS, and the patient complained of severe visual compromises.
- On imaging, atrophy appeared to be affecting the fovea more clearly (Figures 5 and 6).
CAUTION: Spoilers ahead!
Finish the interactive case before reading the synopsis below.
Summary/Clinical Take-Home
This case exemplifies a typical case of advanced AMD with the right eye being treated for wet AMD and the fellow left eye showing atrophic changes that went on to rapidly affect the foveal center.
GA patients regularly complain of worsening vision, which, when evaluated, show little change under high contrast conditions. If visual acuity is evaluated under low luminance conditions, a large drop in vision is often detected. This is because the foveal center appears to be spared at the beginning of the disease process, but it is affected in a subtle way by losing contrast vision, which affects daily activities. Unfortunately, this patient went from being an active and independent person to a fearful, depressed, and dependent person due to poor vision. During a recent visit, she mentioned that she feels like a burden to those caring for her.
GA progression should be evaluated regularly to try to establish speed of progression. All treatment options need to be discussed with patients so they can make an informed choice.

Patricio G. Schlottmann, MD
- Director of the Research Department, Charles Ophthalmic Center
- Ophthalmology Department Director at Organización Médica de Investigación in Buenos Aires, Argentina
- Financial Disclosure: Consultant (4DMT, AbbVie, Adverum, EyeBio/Merck, EyePoint, Horizon Surgical, Novartis, Ocular Therapeutix, Oculis, Roche/Genentech)