This Case Report is Interactive!
Strengthen your understanding of geographic atrophy by answering the challenge questions below.
Case Presentation
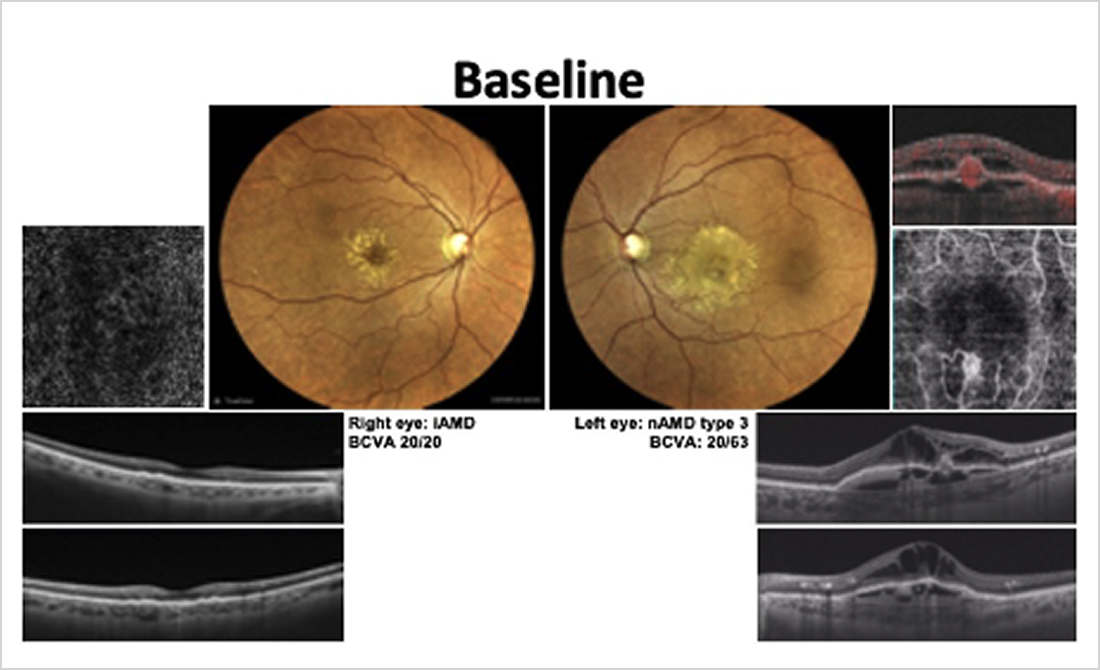
A 74-year-old White female was referred to our clinic for evaluation and management of newly diagnosed neovascular AMD (nAMD) in the left eye (OS), characterized by a retinal angiomatous proliferation (type 3 macular neovascularization [MNV]). At presentation, the patient reported the recent onset of metamorphopsia and blurred vision OS. The right eye (OD) had no symptoms but was monitored, given known bilateral drusen.
- The patient is an ex-smoker with no family history of AMD and has blue irises.
- Risk factors included age, light iris color, and past smoking history.
- Relevant systemic conditions included well-controlled hypertension and hypercholesterolemia. She was on a statin and an ACE inhibitor.
The patient’s BCVA was 20/20 OD and 20/63 OS. The left eye showed intraretinal hemorrhage and intraretinal fluid, with pigment epithelium detachment consistent with type 3 MNV, as shown by color fundus photography, structural OCT, and OCT angiography (Figure 1). The right eye showed medium-to-large soft drusen with no signs of exudation. Swept-source OCT (SS-OCT) showed multiple confluent drusen and mild retinal pigment epithelium (RPE) irregularity, with preserved outer retinal layers. No signs of complete RPE and outer retinal atrophy (cRORA) or MNV were detected in the right eye. The patient was diagnosed with active exudative AMD OS and intermediate AMD OD.
Challenge Question 1/2
True or False: Neovascular age-related macular degeneration (nAMD) and geographic atrophy (GA) cannot co-exist in the same eye.
Answer the question above to reveal more case details.


Correct answer: B. False
The patient began intravitreal anti-VEGF treatment in the left eye. For the right eye, AREDS2 supplementation was recommended, along with lifestyle counseling (smoking abstinence, UV protection). The visual prognosis was discussed. She was informed about the risk of progression to GA and the need for ongoing surveillance.
Challenge Question 2/2
Which of the following statements about the relationship between BCVA and geographic atrophy (GA) progression is most true?
Answer the question above to reveal more case details.


Correct answer: D. There is no known correlation between visual acuity and prognosis for GA progression
The patient has since been followed for 10 years for continued monitoring of the right eye (observation with semiannual SD-OCT, fundus autofluorescence, fundus photography, and BCVA monitoring) and treatment of the left eye (continuation of anti-VEGF injections as needed based on disease activity). In the right eye, serial multimodal imaging revealed the following evolution (Figure 2):
- Years 1–5: Gradual enlargement and confluence of drusen with localized RPE elevation;
- Year 8: Spontaneous regression of drusen in the perifoveal region;
- Year 10: Development of parafoveal cRORA lesions consistent with GA, while foveal structure and BCVA remained preserved;
- VA remained stable at 20/25 OD.
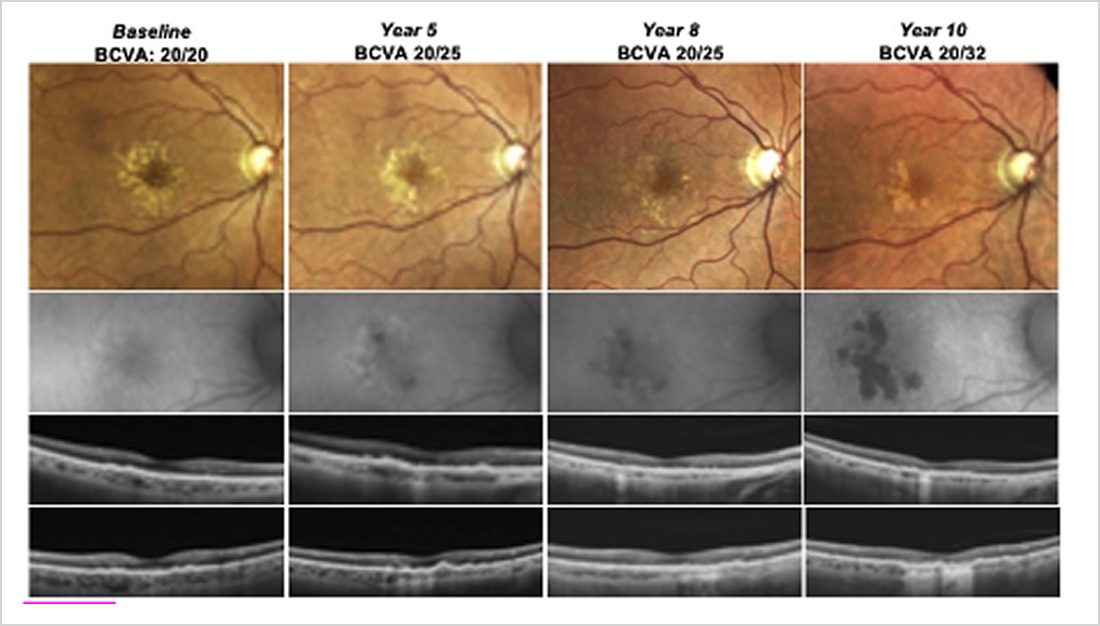
Figure 2. Multimodal imaging of the patient’s right eye captured over a 10-year period. Fundus autofluorescence (FAF) imaging showed sharply demarcated hypoautofluorescent areas consistent with geographic atrophy. OCT demonstrated outer retinal thinning and hypertransmission through Bruch membrane in atrophic areas.
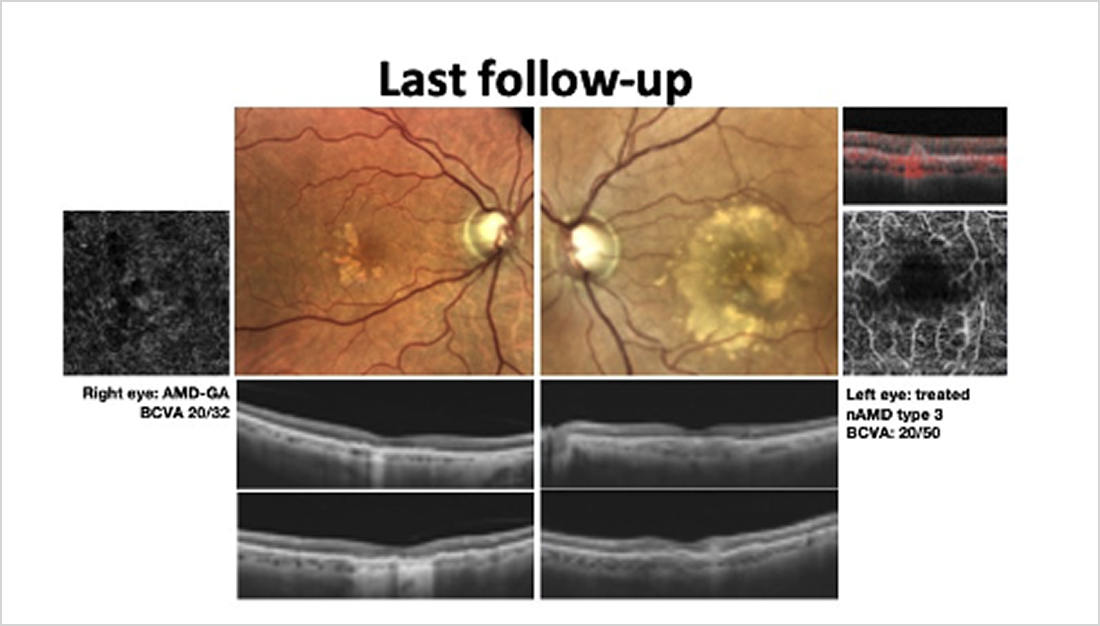
At the most recent follow-up, the right eye had preserved central vision (BCVA 20/25), with foveal-sparing GA and no signs of MNV conversion. The left eye remained stable under anti-VEGF therapy (Figure 3).
CAUTION: Spoilers ahead!
Finish the interactive case before reading the synopsis below.
Discussion
This case highlights the typical evolution of intermediate AMD in a high-risk fellow eye of a patient with unilateral type 3 neovascular AMD. Over a decade of follow-up, the right eye progressed from soft drusen to confluent drusen, followed by spontaneous regression and the insidious development of parafoveal GA. This sequence reflects a well-documented natural history of GA, where structural deterioration may occur despite stable central vision.
Importantly, sparing of the fovea allowed functional preservation. The patient’s consistent follow-up, adherence to preventive measures (AREDS2, UV protection, smoking cessation), and early counseling contributed to proactive care and reduced anxiety related to progression. This case reinforces the value of longitudinal multimodal imaging, particularly OCT, in anticipating functional risk and informing management—even in asymptomatic eyes.