This Case Report is Interactive!
Strengthen your understanding of geographic atrophy by answering the challenge questions below.
Case Presentation
A 73-year-old Caucasian female was referred to our clinic for evaluation and management of newly diagnosed neovascular age-related macular degeneration (nAMD) in the right eye (OD), characterized by retinal angiomatous proliferation (type 3 macular neovascularization [MNV]). At presentation, the patient reported a recent onset of metamorphopsia and blurred vision OD. The left eye (OS) was asymptomatic but monitored due to known bilateral reticular pseudodrusen.
- The patient is an ex-smoker and reported that her sister lost vision bilaterally due to AMD. She has brown eyes.
- GA risk factors identified included age, family history, and past smoking history.
- Relevant systemic conditions included well-controlled hypertension and hypercholesterolemia. She was on a statin and a beta-blocker.
BCVA was 20/40 OD and 20/20 OS. The right eye showed small intraretinal hemorrhage and intraretinal fluid with retinal pigment epithelium (RPE) detachment consistent with type 3 MNV, as demonstrated by structural OCT, fluorescein angiography, and indocyanine green angiography (Figure 1). The left eye showed reticular pseudodrusen without signs of exudation. No signs of complete RPE and outer retinal atrophy (cRORA) or MNV were detected in the left eye.
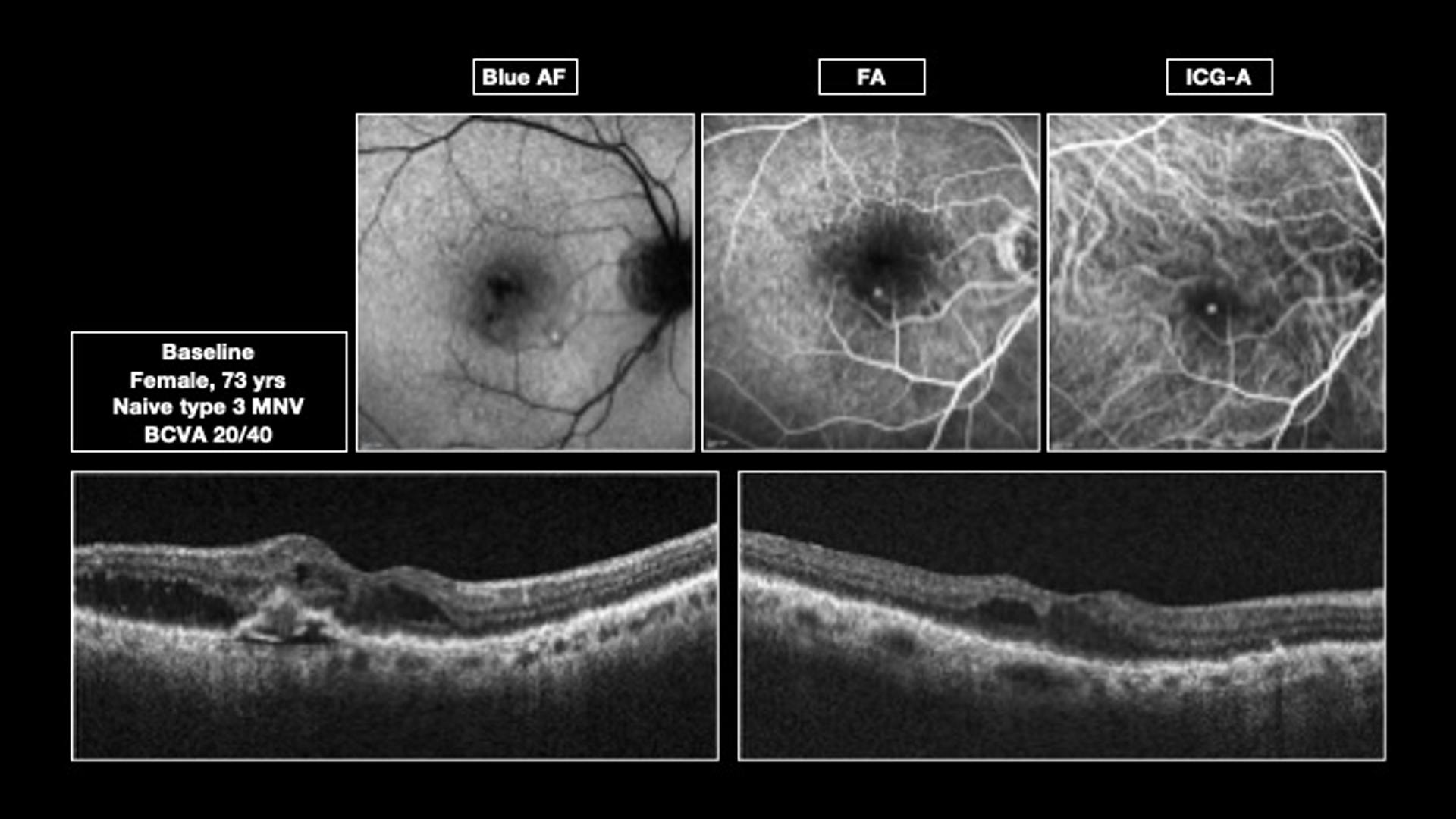
Figure 1. Multiple imaging views of the patient’s right eye at presentation confirmed the presence of type 3 macular neovascularization.
Challenge Question 1/2
Which of the following statements is most true regarding reticular pseudodrusen and risk of geographic atrophy (GA):
Answer the question above to reveal more case details.


Answer: C. Presence of reticular pseudodrusen has been associated both with the development of new GA lesions and with risk for faster growth of existing lesions
Management Plan and Counseling
The patient began intravitreal ranibizumab (Lucentis, Novartis) treatment in the right eye, and AREDS2 supplementation was recommended along with lifestyle counseling (smoking abstinence, UV protection). The visual prognosis was discussed. She was informed about the bilateral risk of geographic atrophy (GA) development.
The patient was followed for 10 years for intravitreal ranibizumab administration in the right eye and for continued monitoring of the left eye. In the right eye, the patient received 20 intravitreal ranibizumab injections over the course of 10 years. The left eye never developed nAMD during the follow-up period. Serial fundus autofluorescence (FAF) showed the following progression (Figure 2):
- Baseline: Neither eye showed signs of GA. FAF revealed reticular pseudodrusen, a distinct type of deposit located above the RPE, appearing as hypoautofluorescent lesions arranged in a reticular or network-like pattern, more prominent in the superior macula.
- Year 1: In both eyes, reticular pseudodrusen became more prominent and were associated with small areas of GA, visible as hypoautofluorescent patches in the superior macula, more pronounced in the right eye.
- Years 3-10: FAF imaging revealed sharply demarcated hypoautofluorescent areas consistent with GA, progressively enlarging and becoming confluent in a typical symmetric annular pattern.
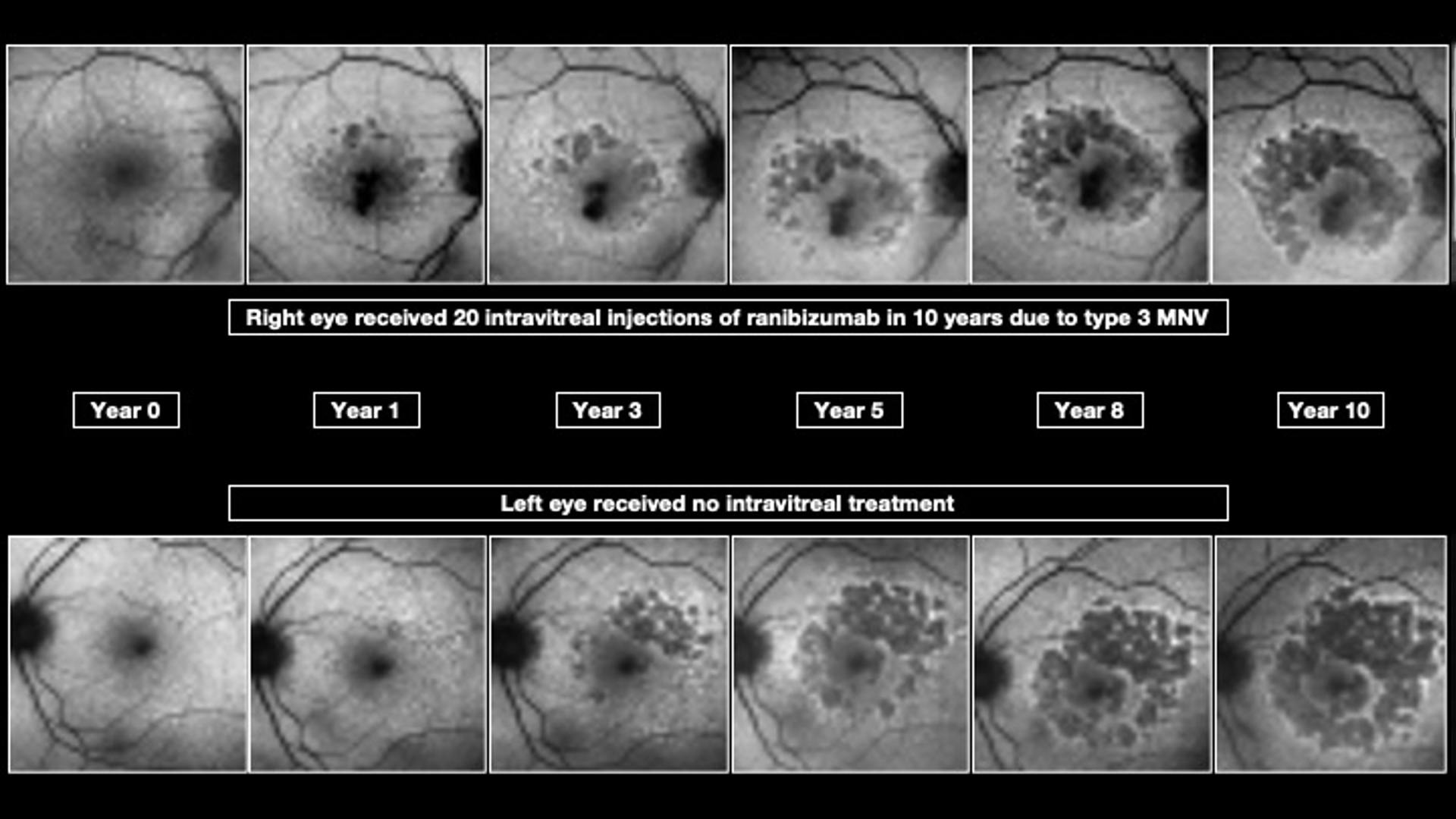
Figure 2. Serial fundus autofluorescence of the patient’s right and left eyes over a 10-year period.
Challenge Question 2/2
What is the significance of hyperautofluoscence as seen on fundus autofluoresence (FAF) imaging?
Answer the question above to reveal more case details.


Answer: B. These lighter areas at the lesion margin indicate zones to which lesions may expand
The long-term treatment plan for this patient was as follows:
- OD: Continuation of anti-VEGF injections as needed based on disease activity.
- OS: No treatment required. Observation with OCT, FAF, fundus photography, and BCVA monitoring.
At the most recent follow-up, the right eye remained stable under anti-VEGF therapy and showed relatively preserved central vision (BCVA 20/40) due to foveal sparing from GA, with no signs of MNV reactivation. OS showed symmetric foveal-sparing GA with no signs of nAMD conversion (BCVA 20/63).
CAUTION: Spoilers ahead!
Finish the interactive case before reading the synopsis below.
Discussion
This case illustrates several key aspects in the natural history and management of GA in the setting of type 3 MNV and reticular pseudodrusen. First, the presence of reticular pseudodrusen is a well-recognized risk factor for GA development, with a characteristic topographic pattern. In this patient, GA initially appeared in the superior and temporal macula—precisely where reticular pseudodrusen was most prominent—and gradually enlarged and coalesced into a symmetric annular configuration. This distribution is consistent with previous studies showing that reticular pseudodrusen-associated atrophy often originates in perifoveal zones, particularly in areas of highest pseudodrusen density. Notably, the progression pattern was symmetric across both eyes, although the onset was not strictly synchronous—a phenomenon frequently observed in bilateral GA evolution.
A second relevant point concerns the debated role of anti-VEGF therapy in GA progression. For years, the potential atrophic effects of chronic VEGF inhibition have been discussed, particularly in the context of long-term treatment for nAMD. In this case, despite one eye receiving 20 intravitreal ranibizumab injections over a decade and the fellow eye receiving none, both eyes exhibited a remarkably parallel and symmetric evolution of GA. This observation adds to the growing body of evidence suggesting that intrinsic patient-specific and disease-related factors—such as age, reticular pseudodrusen burden, genetic predisposition, and baseline choroidal thinning—may play a more dominant role in GA pathogenesis than anti-VEGF exposure.
Furthermore, the preservation of central vision in both eyes, despite extensive perifoveal atrophy, underscores the functional significance of foveal sparing. This highlights the importance of regular imaging not only to detect and monitor atrophic changes, but also to identify risk to the fovea early, enabling timely counseling and adaptation of care strategies.
Overall, this case reinforces the importance of longitudinal follow-up in AMD patients with reticular pseudodrusen, even in the absence of exudative activity, and supports the notion that GA development is a multifactorial process not accelerated by anti-VEGF treatment.