The following case study is the fourth in a series of cases that have highlighted treatment intervention with LACRIFILL Canalicular Gel (Nordic Pharma, Inc.). Here, an existing patient with dry eye disease (DED) presented with indications of Demodex blepharitis infestation that worsened her quality of vision and contributed to her DED.
Presentation
In July 2020, a 68-year-old woman with a medical history of high cholesterol, cataracts, and long COVID with sleep apnea presented to me with complaints of ocular burning and dryness that worsened throughout the day. Both eyes were equally affected. The patient's osmolarity measured 294/304, which was a significant differential of 10. Her bilateral UCVA was 20/20. I first confirmed her sleep apnea was well controlled. I diagnosed her with DED and placed her on an immunomodulator, after which her osmolarity leveled out to 295/291. I have followed her for many years, during which she continued the treatment of lifitegrast and we added varenicline twice a day along the way to increase her production of natural tears. Her symptoms remained stable for a few years.
In September 2024, the patient returned to me with additional symptoms of itching and discomfort upon wakening indicative of Demodex blepharitis infestation. She did have collarettes evident on all 4 lids at the slit-lamp exam. Her SPEED questionnaire measured 8/28, which is clinically meaningful, and I moved forward with treating her Demodex blepharitis. I initiated lotilaner ophthalmic solution 0.25% BID for 6 weeks along with a gentle lid hygiene regimen.
Treatment
As discussed with the new diagnosis of Demodex blepharitis, I placed the patient on XDEMVY (lotilaner ophthalmic solution) twice daily for 6 weeks. This cleared her Demodex blepharitis infestation but because of this comorbidity it had exacerbated her existing DED to an uncontrollable level. At her follow-up visit in October 2024, the patient's osmolarity was still normal, but her SPEED questionnaire measured 10/28, and I found significant inferior corneal staining as well as a low tear meniscus height (TMH). It was at this visit that I instilled LACRIFILL Canalicular Gel at 0.1 mL per puncta. She has a connected canalicular system, meaning that I only had to place the cannula in the lower puncta to achieve a full fill of the lower and upper canalicular system. Clinically, the only way to know that this system is connected is by regurgitation of the gel through the upper puncta while filling the lower puncta (Figure).
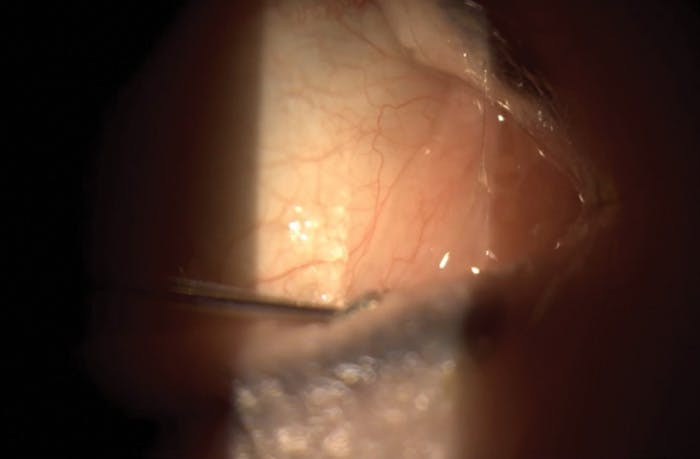
Figure. Instillation of LACRIFILL Canalicular Gel was determined necessary upon the patient’s follow-up visit.
Outcomes
When the patient returned 4 weeks later following LACRIFILL Canalicular Gel placement in all 4 puncta, her vision remained 20/20 in both eyes and her osmolarity measured 296/290. Furthermore, her SPEED questionnaire had improved to 5/28, and the inferior corneal staining had reduced to minimal punctate staining. The patient's tear break-up time (TBUT) measured 10 seconds OD and 11 seconds OS, and her tear meniscus height was 0.35 mm and 0.27 mm respectively. This patient did not experience any adverse events or complications following LACRIFILL Canalicular Gel placement.
Conclusion
This case exemplifies the successful management of a patient whose chronic, stable DED became acutely exacerbated following necessary treatment for a Demodex blepharitis infestation. Both the patient and I were very pleased with the results achieved after the placement of LACRIFILL Canalicular Gel. The significant improvement in her SPEED score from 10/28 to 5/28, coupled with the resolution of significant inferior corneal staining to minimal levels, and her increase in TMH demonstrated a marked recovery of her ocular surface health. I believe LACRIFILL Canalicular Gel was the optimal treatment strategy at that juncture because her DED had become uncontrollable with her prior regimen after the Demodex treatment. LACRIFILL Canalicular Gel provided immediate and sustained tear conservation by blocking tear outflow, effectively increasing her tear volume on the ocular surface as demonstrated by the TMH. This directly addressed the heightened dryness, discomfort, and corneal staining the patient experienced.1
What proved most challenging in this case was managing the delicate interplay between two distinct ocular surface conditions. Successfully eradicating the Demodex infestation was crucial, yet it simultaneously destabilized her underlying DED, requiring a swift and effective secondary intervention. We are sometimes challenged clinically when patients who have been well managed decompensate. It is incumbent upon us to understand that her current treatment hadn’t stopped working; the patient had a new disease state that needed to be addressed. It was particularly interesting to observe how profoundly the Demodex blepharitis impacted her DED status and, conversely, how effectively LACRIFILL Canalicular Gel restored stability after successfully treating her Demodex blepharitis infestation. Following her successful LACRIFILL Canalicular Gel treatment, I continue to monitor her condition closely with follow-up visits every 3 to 4 months. Of note, most recently along this journey she has developed significant cataracts OU and now needs cataract surgery. Fortunately for her, she has an ocular surface that is now optimized, clearing the path for her upcoming cataract surgery consultation without delay.
1. Packer M, Lindstrom R, Thompson V, et al. Effectiveness and safety of a novel crosslinked hyaluronate canalicular gel occlusive device for dry eye. J Cataract Refract Surg. 2024 1;50(10):1051-1057.



